Live Gastric Band Surgery
Read more about the gastric band surgery by Dr Nagi Safa
Gastric band surgery or Laparoscopic Adjustable Gastric Band is used to restrict your food consumption so you can lose weight. You eat a smaller volume of food and your stomach fills up quickly. You still need to make the right choices in the food you eat to reduce calories in the diet. If exercise is added to the routine weight loss can increase even further. There are two main brands of lap bands which used. The FDA or Food and Drug Administration approves these bands for weight loss. These bands are a modification of the Vertical Banded Gastroplasty procedure which isn’t used as much in the United States because of the lack of long-term success and the high rate of complications after surgery. The bands used in the Vertical Banded Gastroplasty procedure are all of the same size and not adjustable after being inserted and the stomach needed to be stapled and cut. The “one size fits all” approach didn’t work as the size and thickness of a person’s stomach varies a great deal. Some bands produced too much tightness and there was acid reflux as well as issues with vomiting. The cutting and stapling of the stomach in the procedure increases leaks and infections and produces poor weight loss results. Since it changes the anatomy of the stomach, conversions or revisions of the surgery are difficult.
Gastric band surgery Placement
In low risk patients, bands can be inserted in outpatient surgery as well as in a hospital setting with an overnight stay. The Surgery should be discussed with your doctor prior to having the work done. Your health. BMI and age will be factors in determining if the surgery is right for you. There can be issues with vomiting as well as nausea after the surgery which may require a hospital stay. A patient will undergo preoperative testing as well as registration before the morning that the surgery is to be completed. On the morning the surgery is to be done, the antibiotics are given to prevent infections. Compression boots and blood thinners are used to prevent blood clots.
For the procedure the patient is given a general anesthesia. There are 6 small incisions and a port is placed in the mid abdomen in the right where the rectus muscle is. The size of the patient’s stomach as well as fat around the area will determine what band is used during the surgery. Man and those with a larger BMI usually get the Allergan© AP large band. Women and those with a smaller BMI get the Realize© C band. Or the Allergan© AP standard band. There is a difference in the length of the bands but the band volume, width, and surgery outcome of the different bands don’t make that much of a difference in instances of complications or the amount of weight loss. All these bands perform around the same.
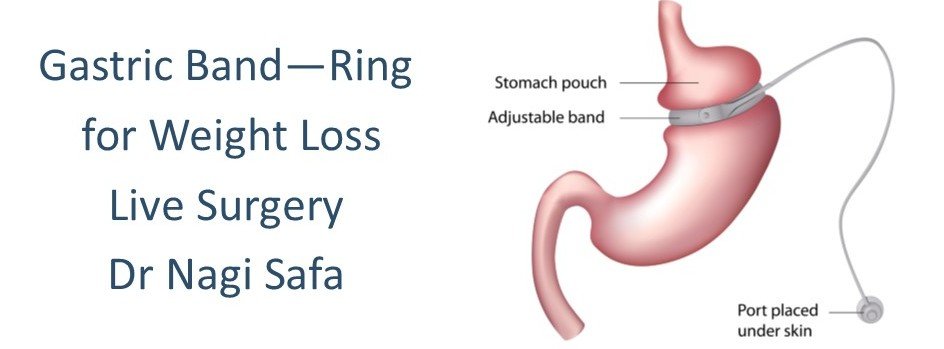
The area by the esophagus and upper stomach and inspected for hiatal hernia before the Laparoscopic Adjustable Gastric Band is inserted. The hernia must be repaired first which prevent the LAGB from moving into the chest which makes the band function poorly. Behind the upper stomach a tunnel is made and the band is then placed around the stomach just like a belt which creates a small 20cc pouch that has a narrowed outlet. A sizing balloon is used to ensure the pouch is always the correct size. The balloon is paced at the top of the stomach and the band is placed around the bottom of the balloon and the pouch. The balloon is then removed and the band is held there with some sutures placed in the stomach wall so there’s no slippage that occurs. The inner part of the band has an adjustable balloon which can be emptied or filled to change the size of the outlet. This is done by in injecting saline into a reservoir which is placed under the skin of the abdominal wall during surgery. IV tubing is used to connect this to the band. The LAGB outlet is tightened in about 3-4 months. The pouch will fill quickly with reduced food amount and then it empties slowly to relive a patient’s hunger. If a patient overeats there is vomiting or pain that will occur.
When the band is first inserted there’s no fluid place din the band until after 30 days during the first post-operation visit. This reduces slippage and post-op vomiting issues. The patient has a Gastroscopic Exam in the OR room where a light is put into the stomach and esophagus to inspect the positioning of the band. This is done to make sure there’s no perforations or leaks in the stomach area and that the band is wide open. A patient is given a liquid diet and usually sent home in 1-4 hours and given medications which they take for 5-7 days. If the patient needs a room they stay overnight to make sure they can tolerate liquids as well as medications without instances of nausea. In the morning an upper GI x-ray is given se see how the band is and that there’s no obstructions or leaks. A patient is sent home and given medication. A stomach acid inhibitor is usually prescribed to help prevent ulcers while the patient heals.
Once off the pain medication a patient can walk and drive, but must not lift over 25 pounds for 3 weeks. Once the 3 weeks are up there’s no restrictions for the patient. For up to 6 weeks there may be some pain present which can be controlled with regular pain medications such as Tylenol. The patient has 6 small meals and protein supplements for 1 week. As the swelling goes down the patient has soft foods like eggs, fish, and cooked vegetables. After 3 weeks the patient can eat regular food, but must make wise food choice like fruit, vegetables, and meat. High calorie liquids, simple carbohydrates, soups, mushy foods, and all junk foods must be avoided.
Three times per week the patient must do aerobic exercise for 45 minutes each session to increase the pulse rate. The patient will go back to the doctor’s office or the hospital every 3-4 months and have the band filled slowly so scar tissue can form which holds the band in place. This helps the patient adjust to the gastric constriction and minimizes instances of vomiting. Some fills are done under fluoroscopic x-ray control in the hospital along with an X-ray to determine the correct outlet size. A patient goes every six months and then one year for a checkup. After that the patient will go once per year and there may be a need for small adjustments as well as fills to make sure the patient is in good health. Supplements like calcium, vitamin D as well as multivitamins can help patients maintain good health of the gastrointestinal tract.
Gastric band surgery benefits and Risks
Risks
- Slippage can occur around the stomach which results in an incorrect positioning of the band and lead to consistent vomiting. The blood supply to the stomach can be interfered with and a perforation can occur. A part of the stomach may die as a result. A reoperation or deflation of the band may need to be performed to remove, revise or put the band in a new position.
- The band may erode into the stomach and cause an infection which requires the removal of the band and a repair of the gastric perforation that occurred. If a patent takes drugs like NSAIDS, steroids, on aspirin these should be avoided after the surgery as they can cause perforation.
- There may be problems with the tubing or port which needs a reoperation to correct the problem.
- A person may have esophageal dilatation which leads to problems with swallowing and the band will need to be removed.
- There may be a medical malfunction of the actual band which can cause problems.
- A patient may have chronic vomiting, acid reflux or might not tolerate the band well. Many people with GERD or Gastroesophageal Reflux Disease have improvements after the surgery while others have complications with it. Some people can’t tolerate the band and may have difficulty swallowing, chronic vomiting or severe pain and need the band removed.
- A person can still drink high calorie liquids or sweets and gain weight. The LAGB only works if the patient lives a healthy lifestyle, exercises, and watches what they eat.
- The band isn’t a permanent solution.
- There’s a need for fluid adjustment sin the hospital or a physician’s office which can consume time which may impact work needs.
Over the past 11 years the LAGB has gone through a lot of changes. The original band was narrower and held only 4cc of saline. This band was tightened right away in the operating room. The band was against the stomach and there were more erosions and slippages that occurred. There was also more instances of vomiting which further increased slippages. The narrow bands increased pressure on the wall of the stomach and adjustments to it were difficult to make. The early bands had 3% erosions and slippage of about 10%.
Now due to improvements there are only about 5% slippages and there’s about 1% erosions after the surgery is done. The band is now inserted away from the stomach wall and there’s fibrous tissue and fat from the upper stomach used to reduce erosions and slips. The bands now form scar tissue better and are left empty in the operating room to reduce vomiting. Over several months the bands are filled slowly so the patient get used to the restrictions that the band produces. The bands are also pre-shaped and are made longer to improve contact with the stomach and to reduce pressure which decreases the risk of erosion.
About 25% of patients that have this surgery will have it removed because of complications, band intolerance, weight loss failure, and slippages. The band wears out in about 15-20 years and needs to be replaced. The patient can leave the band, but it will not function or have the band replaced. There is also the option of having another type of weight loss surgery.
Benefits
There are benefits to the gastric band surgery when you compare it to Roux En Y Gastric Bypass, Vertical Banded Gastroplasty, and the Sleeve Gastrectomy procedures.
- There’s no cutting or stapling of the stomach so this reduces infections and leaks. This is the safest weight loss surgery that’s currently available. There’s a 0.10% or 1/1000 chance of dying during this procedure. With the other procedures the risk is greater at 0.05% or 1/200 chance.
- The band can be tightened or loosened so there’s improved weight loss and less issues with vomiting. These adjustments can be mad years after the procedure and the patient can still lose weight if they following guidelines and maintain a healthy lifestyle.
- Since there’s no cutting or stapling of the stomach the procedure is reversible with less scarring.
- Losing as little as 10% of body weight can improve the patient’s health. About 65% of those that have to done have reduction or resolution in diabetes, hyperlipidemia, hypertension, acid reflux, sleep apnea, and issues with their joints. A patient does have to lose weight to see improvements, but the band can help facilitate this.
Outcome of the gastric band surgery
Patients tend to lose about 50% of their excess weight and are about 50% successful over the longer term which means they keep the weight off over 5 years this has been shown in clinical trials and studies.
Why Should a Person Consider Getting a gastric band surgery?
If a person has a BMI less than 5 the band is ideal. The closer the patient is to being about 100 pounds or less over their ideal body weight then the more chance they have for success. People that like big meals, but don’t eat junk food all day long will have success as long as the meals are healthy they eat a lot and get full quickly. The discomfort of the band keeps them from eating more. People with a sweet tooth will do poorly as they tend to take in far too may simple carbohydrates like chips, cookies, and ice cream. These people don’t overeat so they don’t tend to notice they have the band on. Since there’s no constriction they don’t benefit from losing weight as they keep eating. They consume calories all day long and this adds up even though they have a band. The small “snacks” add up to large amounts of calories.
For the band to work, calories must be restricted to 1200 per day. This can be accomplished worth better food choices which have fewer calories, but still make you full. Junk foods are dense with calories, but don’t fill you like real food does.
A person that has a BMI over 50 or weigh 350 pounds or more are generally not happy with the weight loss they get from the band.